Measuring the cost of performed services has long been challenging for healthcare providers. Healthcare is both a high volume and high uniqueness/complexity industry. Additionally, healthcare delivery is not a two-party transaction. Several layers of both private and public entities (e.g., hospital corporations, governments, insurance companies, and pharmaceutical companies) exist between the service providers, such as the physician and the customer - the patient. Further, having a unified automated repository to merge the direct, semi-direct, and indirect contributors of cost and then calculate the costs based on a methodology that can get to the encounter level of detail has been a challenge. Healthcare data can reside in separate silos, impeding insight and making data-driven decision-making difficult. Revenue cycle optimization becomes complex when disparate systems lack integration, making tracking financial performance across entities harder. Existing solutions have been created but have been expensive to build (or acquire) and maintain, with overall high integration and support costs. As healthcare systems evolve, adopting scalable costing solutions is essential to ensure sustainable financial management and improved performance.
A scalable cost solution is needed as much as ever, and its importance will continue to grow. Whereas healthcare financial planning has historically been based on a fee-for-service arrangement, it may no longer be so. The cost model has often not provided an actual cost per service but rather a ratio or factor based on the expected revenue. As the industry moves away from the pure fee-for-service model into fixed fee, capitation, or lump-sum payment arrangements, (revenue)-based costing practices, which were never highly accurate, become even less meaningful for healthcare cost management and revenue cycle optimization.
Alithya has developed several pre-built accelerators and solutions in healthcare to meet multiple needs, including Alithya Cost of Care Analytics for healthcare systems.
Alithya Cost of Care Analytics for health
Built upon Alithya’s healthcare data foundation model and leveraging the power of Oracle’s Enterprise Profitability and Cost Management (EPCM), this offering combines patient billing and encounters, provider data, payor data, and financials. The solution allocates and assesses revenue and costs to individual encounters to enable diverse reporting opportunities. It also provides the ability to perform scenario analysis that can support multiple methodologies, including, but not limited to, the ratio of costs to charges (RCC), relative value units (RVU), and activity-based costing (ABC). In so doing, users obtain quick value with 200 KPIs and 40 visualizations, integrating with existing data sources such as general ledger, contracts, claims, electronic medical records (EMR), and billing – enhancing operational efficiency and financial transparency. These results are reflected in the leading cloud-based healthcare analytics tool, Fusion Data Intelligence Platform (FDIP).
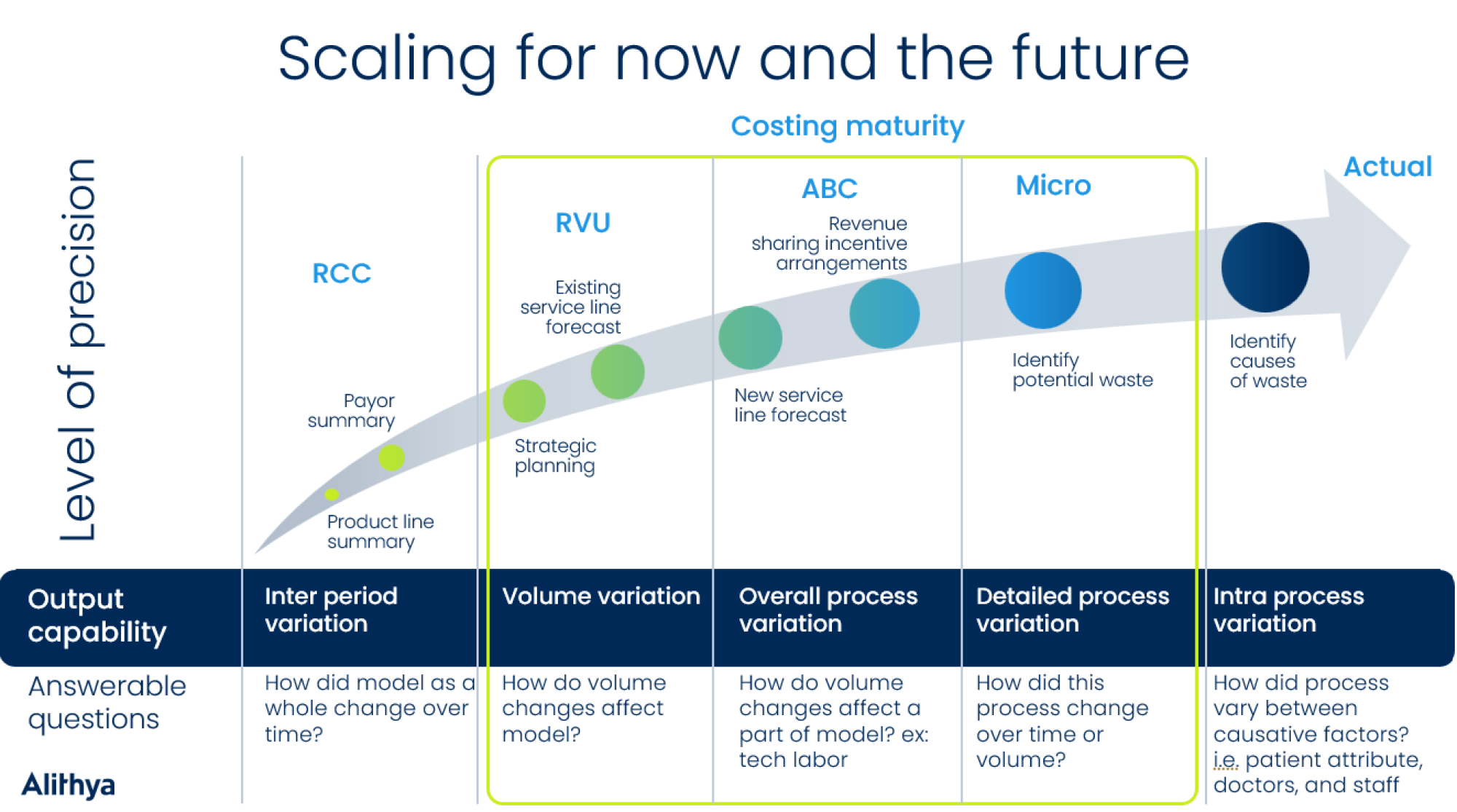
A key component to making the solution viable is that it needs to be scalable. In this context, “scalable” applies not only to its ability to grow in scope but also its ability to evolve from a methodology perspective. The solution must be useful now, even if only limited data is available at an organization. Yet, the foundation for the future must be laid up-front so that, as more sophisticated and accurate methods are pursued, the system can be updated with limited intervention and effort, be able to continue to operate, and be of ever-increasing value.
The ability to accommodate multiple methodologies initially and over time relates to the “Costing Maturity” curve, shown below, which has been established to depict this journey.
Costing methodologies: RCC, RVU, and ABC
The ratio of cost to charges (RCC) method shown toward the beginning of the curve assumes a linear relationship between the cost of a procedure or service and the amount for which the service can be charged to the payer. Such a method ignores any variation or complexity of a service based on the actual resources utilized. It is a de facto revenue-based allocation that can be more straightforward to implement, but it provides less insight into the real cost drivers of providing care. As effective healthcare cost management becomes more critical, organizations seek methods that improve cost accuracy and transparency.
Moving along the path, the next commonly utilized method is the relative value units (RVU) method. This approach employs a weighted volume method for allocation, in which the weightings are complex factors. These factors are based on data that has been collected locally or from broader standards, such as the relative consumption of resources, including labor, supplies, and equipment. The allocation driver is the volume of service performed, multiplied by this factor. This approach is a directionally improved method for understanding costs and profitability of charge items and encounters and, ultimately, lines of service. Additionally, it provides predictive analytics capabilities by identifying patterns in resource utilization, helping organizations adjust their financial planning strategies.
As healthcare payment models evolve, methods like RVU and ABC play a crucial role in ensuring performance-based reimbursement, aligning cost structures with patient outcomes and value-driven care initiatives.
Further up the curve lies the activity-based costing (ABC) approach. Under this methodology, the “causality principle” is developed in which expenses are first assigned into groups of resources performing like activities. The costs of these resources are transferred to the major activities of direct and indirect departments based on appropriate drivers. Hours by job category or specific outputs, such as the number of tests, can be used for cost drivers. This transforms the financial view of an organization into a process-based view, which helps identify improvement opportunities and ensure cost transparency. These process-based costs can then be allocated to charge codes based on additionally identified relevant drivers. While ABC provides data-driven insights, creating and maintaining is a more data-intensive process.
The evolution to real-time, actual costing with micro-costing
Near the top of the upper right side of the curve lies the more advanced concept of micro-costing. Under the prior approaches, RCC, RVU, or ABC results are calculated from the bottom-up at relatively aggregated levels of detail, such as a procedure or charge codes. With a micro-costing approach, these are converted into unit cost rates that are applied in a “top-down” manner to very granular levels, such as patients or encounters, which number in the hundreds of thousands or even millions. This enables real-time cost analysis, offering a deeper understanding of financial implications across services.
Further development of micro-costing involves applying advanced bottom-up methodologies from the start of the process to the encounter level. This approach enhances cost accuracy and provides a more precise financial picture, aligning with value-based care models that prioritize efficiency and patient outcomes.
In both the bottom-up/top-down and all bottom-up approaches, costs are assigned to charge codes based on their relative consumption of resources with equal accuracy. However, when going to the encounter level of detail, this is where they can differ. In some cases, a well-derived unit cost and associated volume (top-down) may be sufficient. For example, some services, such as radiological tests (e.g., X-rays, CT scans, MRIs), have uniform costs, which are calculated to factor in specific equipment usage, utilities, and specialized technicians. The resulting standardized unit cost can then be applied across encounters.
On the other hand, complex procedures like surgeries may require encounter-specific adjustments due to patient attributes or co-morbidities. In such cases, a generalized unit cost applied across all encounters would reduce accuracy, with lower-complexity cases subsidizing more complicated ones. This is where micro-costing becomes essential for financial reporting and forecasting.
The final level of costing maturity—depicted as "actual"—leverages AI-driven tracking technology, process mining, and automation to refine cost allocation. Organizations can achieve the highest level of cost accuracy and operational efficiency by integrating data from multiple systems, such as materials management, electronic medical records, timekeeping, contracts, and billing.
Future-ready healthcare costing: scalable, adaptable, and insight-driven
A scalable healthcare costing solution should be useful both immediately as well as in the future, providing improved methods and information insights from what was previously used. Over time, it can be augmented and improved with more advanced methods without having to completely redesign and rebuild the application.
Alithya’s combined experience in cost management and healthcare using Oracle’s leading cloud-based technology in costing, data visualization, and business intelligence all come together with a cost of care solution that supports business requirements and does so in a way that enables organizations to move toward the upper right of the maturity curve at a pace that is suitable to them. Along the way, they can retain or replace methods as they see fit without having to discard existing work or implement new technology. Contact us today to start your healthcare transformation journey.
