Providing healthcare services to a broad segment of the public has been a topic of debate for decades. Yet, in spite of this subject having been central to the national discourse for so long and having experienced many changes, healthcare structurally remains recognizable to that which was in place before multiple generations of the current population were even born.
As far back as 1974, Robert D. Eilers, a national expert in healthcare delivery who pioneered the launch of formal university training in healthcare financing, wrote, “the failure of traditional institutional arrangements to control healthcare costs, and their apparent inability to make care available on a more widespread basis, has caused many to look at new methods of financing and delivering healthcare.”
Nearly fifty years later, the financing of healthcare continues to be a central theme in the debate as to what kind of healthcare system is most desirable. Politicians debate how many trillions of dollars are necessary and then whether society is able or willing or able to spend them. Central to making these financing decisions is an understanding of the underlying costs of medical care, which has been elusive to date.
It is both a surprise and not a surprise that the industry does not have a firm grasp on the underlying costs of its services. No manufacturer of widgets could have survived so long in such a condition. But, a variety of factors make healthcare unique and the situation more understandable. Consider a few such factors as follows.
Barriers to a Costing System in Healthcare vs. Other Industries
1. In industries other than healthcare, organizations will only spend an incremental dollar as long as the incremental return is greater than that dollar, usually further subject to some kind of hurdle rate of return on investment. Simply stated, nobody is going to spend an extra dollar on something if the amount received from that outlay is only 90 cents. However, with healthcare, the tendency is that spending keeps occurring until the patient is cured or expires. The incremental return logic goes out the window.
2. Almost every episode of care is a unique event based on the specifics of the patient, with co-existing conditions, the so-called co-morbidity, that drive its uniqueness. While large volumes of data can generate overall trends, true costs can be as unique as the people themselves that are being treated.
3. Healthcare is not a pure two-party transaction. Several layers of both private and public entities, e.g. hospital corporations, governments, insurance companies, and pharmaceutical companies, to name a few, exist in between the service provider such as the physician, and the customer, the patient.
4. Healthcare has always been a fee for service arrangement, but it may no longer be so in the future. The fees for services, once set by the providers themselves, are now set by the payors, i.e. the insurance companies, so the cost model has often been not so much a true cost per service, but rather some ratio or factor based on the expected revenue. As the industry moves away from the fee for service model into fixed fee or capitation arrangements, this charge-based costing practice becomes less meaningful.
5. Having a unified automated repository to merge all of the direct, semi-direct, and indirect contributors of cost and then calculate the costs based on a methodology, has been a challenge.
- Healthcare data reside in silos, which impede insight and make analytics difficult to deliver.
- Integration complexity adds increasing costs and has made a rapid response to changing needs very difficult, nearly impossible in the view of some.
- Homegrown solutions have been created, but they have been expensive to build and maintain, with overall substantially high integration and support costs.
Yet, the pressure continues. With so many dollars on the line, a slight misstep in a revenue or expense negotiation could make a large difference in whether an organization in its aggregated total earns enough to be economically viable or if it does not. Throw in an unexpected variable, such as a global pandemic, and the situation goes from simply being important, to being an imperative.
Alithya’s Oracle Practice has developed several pre-built accelerators and solutions in Healthcare to meet multiple needs, among which is the cost of care.

Specifically, the cost of care solution enables the allocation of costs with varying methodologies to detailed levels to analyze and understand them.
Built upon Alithya’s Healthcare Data Foundation, combining patient billing and encounters, provider data, payor data, and financials, the cost of care solution allocates and assesses revenue and costs to individual Services, Providers, and Patients. It enables performing scenario analysis comparing multiple methodologies, including, but not limited to, Ratio of Costs to Charges (RCC), Relative Value Units (RVU), and Activity Based Costing (ABC). In so doing, users obtain quick value with 200 KPIs and 40 visualizations, integrating with existing data sources such as General Ledger, Contracts, Claims, Electronic Medical Records (EMR), and billing, to name a few. It surfaces those results in the leading cloud data visualization tool, Oracle Analytics Cloud (OAC).
A key component to making a solution of this type to be viable is the ability to accommodate multiple methodologies that can be facilitated over time. The “Costing Maturity” curve, shown below, has been established as a means to depict this journey.
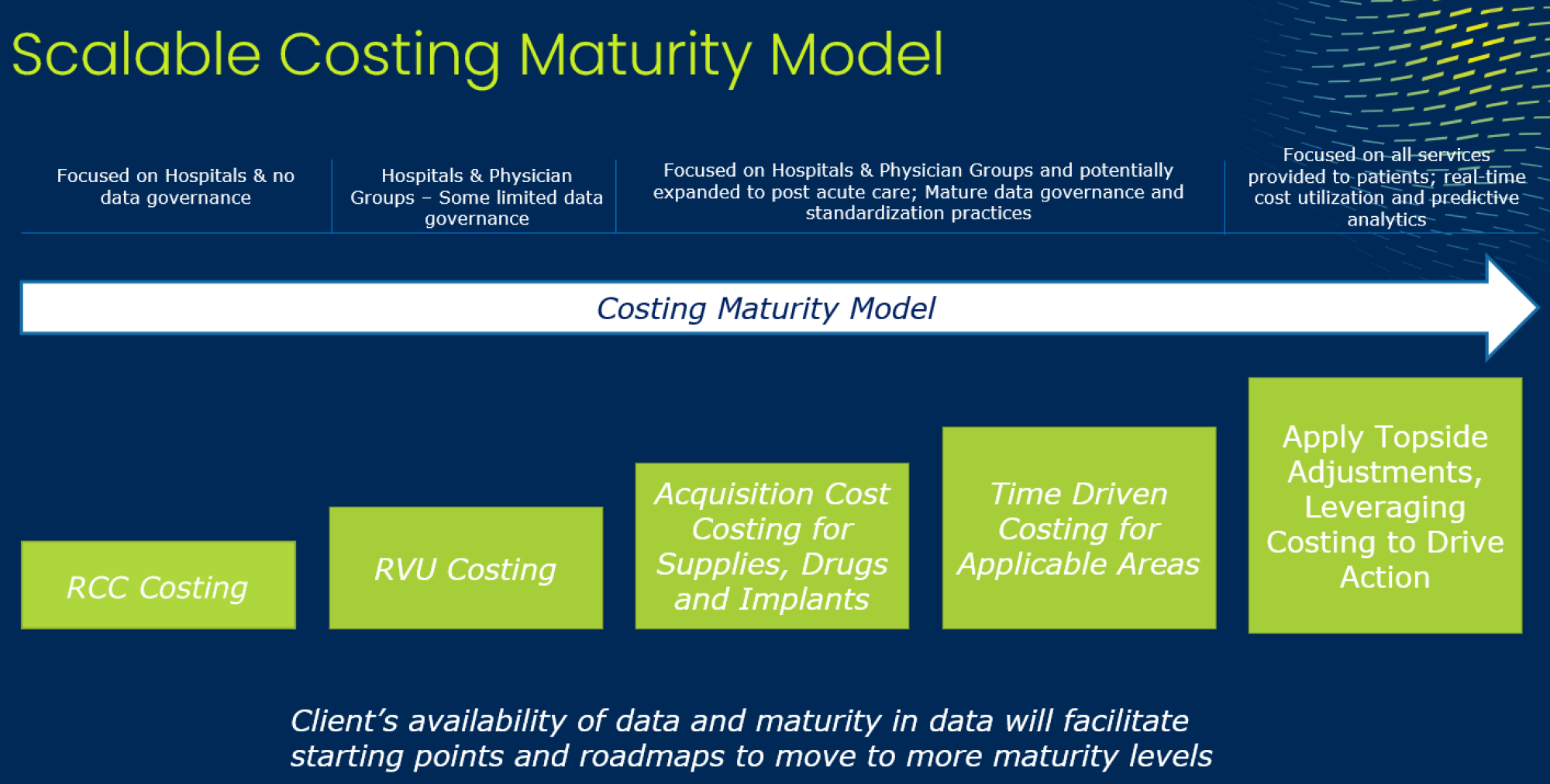
The RCC method toward the beginning of the curve assumes a very linear relationship between the cost of a procedure or service, to the amount for which the service can be charged. Such a method ignores any variation or complexity of a service based on the resources utilized. It is a de-facto revenue-based allocation that may be relatively straight forward to implement, but it provides little insight into the real cost or opportunity for improvement.
Moving along the path, the next commonly utilized method is the RVU method. This method takes actual costs and uses a weighted volume method for allocation, in which the weightings are complexity factors. These factors can be based on the utilization of resources, both physical and financial, and is a directionally improved method for understanding costs and net margin.
Further up the curve lies the Activity Based Costing approach, which has been selectively undertaken in healthcare. Under this methodology, the “causality principle” is developed in which expenses are first assigned into groups of resources performing like activities. The costs of these resources are assigned to the major activities of direct and indirect departments based on appropriate drivers. This transforms the financial view of an organization into a process-based view which helps identify improvement opportunities. These process-based costs can then be allocated to charges and later patient segments or other “cost objects” based on additionally identified relevant drivers. ABC-based costs are far more meaningful than those of other methods, but it can be seen that it is a data-intensive process to create and maintain, and therefore requires robust technologies.
Finally, toward the upper right of the curve, lies the more advanced concept of “microcosting”. Under this approach, RVU or ABC-based results which are calculated from the “bottom-up” at relatively aggregated levels of detail such as procedure or charge codes, are converted into unit cost rates that are applied in a “top-down” manner to very granular levels such as patients or encounters, which number in the hundreds of thousands or even millions. This enables ascertainment of the most detail for the most in-depth analysis.
The above speaks to methods of cost allocation, which combine financial data and operational driver data. However, a cost of care system also needs the capability to further identify direct charges such as material and supplies or payroll. Users want to understand which specific materials were consumed in a procedure such as which surgical adhesive or which fracture repair kit was used, and from what vendors. From a payroll perspective, they may want to understand which types of physicians, nurses, or physical therapists were utilized. As such, these direct charges introduce additional data sources such as materials management, electronic medical records, timekeeping, contracts, or billing.
After considering all of the requirements for a robust cost of care system, perhaps it is no surprise that such systems have been elusive.
Conclusion
Alithya’s combined experience in cost management and healthcare using Oracle’s leading cloud-based technology in costing, data visualization, and business intelligence all come together with a cost of care solution that supports these requirements and does so in a way that enables organizations to move toward the upper right of the maturity curve at a pace that is suitable to them. Along the way, they can retain or replace methods as they see fit without having to discard existing work or implement new technology.
- Finally, consider these types of questions:
- How do my hospital’s services compare across the health system?
- How can I optimize service location? Should I consolidate services?
- What impact to my bottom line will there be if there is a rate change? Can I afford to sign this managed care contract?
- Can I compare my payors’ profitability and score them?
- Am I charging for all the services that I am performing?
- What is my profitability across service lines by hospital?
- Why are the costs for a particular service increasing? Is it due to labor, supplies or is it physician practices-related? How can we decrease these costs?
- Where should I focus my cost reduction initiatives? How do I track success?
If these are the kinds of questions that are being asked, then Alithya’s cost of care solution may provide the answers.
For comments, questions, or suggestions for future topics, please reach out to us at [email protected]. Visit our blog regularly for new posts about Cloud updates and other Oracle Cloud Services such as Planning and Budgeting, Financial Consolidation, Account Reconciliation, and Enterprise Data Management. Follow Alithya on social media for the latest information about EPM, ERP, and Analytics solutions to meet your business needs.
